Cristhian Armenteros1Andrea Odzak1, Florence Arcondo1Marcela Of God Soler2Tatiana Sinigier3, Marcelo Zylberman1
1 Division of Medical Clinic, Hospital General de Agudos Dr. Cosme Argerich,
2 Pathological Anatomy service, Hospital Marie Curie,
3 Plastic surgery, Hospital General de Agudos Dr. Cosme Argerich, Buenos Aires, Argentina
Summary
Connective tissue diseases linked to breast implants silicone have been a topic of discussion. In the last decade, the siliconosis has been included in the syndrome autoimmune/inflammatory induced by adjuvant (ASIA) with the syndrome, Gulf war syndrome, miofascitis macrophagic and phenomena post-vaccine. The ASIA may manifest as lupus, rheumatoid arthritis, or more rarely as adult Still's disease. We present the case of a patient with prolonged fever and clinical criteria compatible with ASIA and Still's disease. We successfully resected the prosthesis and the anatomical pathology ruled out anaplastic lymphoma ALK (-) that is linked to a prosthesis. Physicians should be alert to the emergence of these new entities associated with breast implants silicone.
Key words: Syndrome ASIA; Siliconosis; Still's Disease; Adjuvant; breast Implants.
Abstract
ASIA syndrome: breast implant and Stills disease.
Connective tissue diseases associated with silicone breast implants have been widely discussed. In the last decade, siliconosis has been included in the autoimmune/inflammatory syndrome induced by adjuvants (ASIA) next to Gulf War syndrome, macrophage myofascitis and postvaccination phenomena. The ASIA syndrome may appear as lupus, rheumatoid arthritis, or more rarely, as adult Still''s disease. We discuss the case of a patient with prolonged fever and clinical criteria for ASIA and Still''s disease. The prostheses were resected and pathology showed absence of breast implant associated anaplastic lymphoma ALK (-). Physicians should be alert to these new entities linked to silicone breast implants.
Key words: ASIA syndrome; Silicone; Stills disease; Adjuvant; Breast implants.
Since its adoption, the use of breast implants silicone (IMS) led to suspicion of association with connective tissue diseases (ETC)1. Despite metaánalisis and recent reviews, these suspicions have not been able to be confirmed2. The siliconosis was one of the first diseases known as “induced by adjuvants” and today is included next to the other, within the syndrome of Shoenfeld syndrome or autoimmune/inflammatory induced by adjuvants (ASIA: for its acronym in English)3. We present the case of a patient with siliconosis, which is manifested as adult Still's disease (SA).
Clinical case
Wife of 61 years, who was admitted for fever (39 °C), arthralgia, myalgia, and pain in the anterior aspect of the left hemithorax, seven days of evolution.
Had replacement of breast implant silicone gel-eight years ago by leaking prosthetic. There were two previous hospitalizations for febrile syndrome; the first nine months ago with spontaneous resolution and the second three months prior to this hospitalization where indicated corticosteroid treatment with normalization of the thermocline. Attached of these hospitalizations, the following additional tests: Hct. 33%, MCV 89, GOT, 84 IU/l, GPT 144 IU/l, ALP 115 IU/l, CRP (C-reactive protein) 130 mg/dl, LDH 1350 IU/l. Serology of viral, HIV, ASTHMA (anti-smooth muscle), anti-LKM (anti-microsomes of liver and kidney), FAN (antinuclear antibodies) and anti-DNA negative. Snap, CPK and aldolase normal. Microbial cultures negative. TAC: adenomegalias axillary and bilateral supraclavicular left > 10 mm Splenomegaly (148 mm). Breast prosthesis bilateral thickening of the soft parts periprosthetic on the left breast. Breast ultrasound left: a collection of anechoic of 28 × 6 mm, compatible with seroma.
Biopsy of axillary lymph node left: expansion marked the T-zone and foci of necrosis. Stains (Ziehl-Neelsen, PAS and Giemsa negativaos.
Liver biopsy: liver disease, chronic active, mild. Video endoscopy high and low and transesophageal echocardiogram were normal.
Physical examination on admission: adenopathy axillary left 2 × 2.5 cm, non-painful; rash maculopapular in the lower limbs and trunk, which is exacerbated by the fever spikes. Splenomegaly.
Laboratory: Hct. 34%, GB 15800/mm3, neutrophils 85%, LDH 1581 IU/l, CRP 223 mg/l, ESR 90 mm/h, ferritin > 2000 ng/ml, GOT 64 U/l, GPT 13 U/l. The rest, without particularities.
CT chest: breast prosthesis bilateral thickening and heterogeneity of tissues paraesternales left and liquid periprotésico. Multiple adenomegalias cervical, axillary and chain breast left. Splenomegaly 140 mm
It was decided to removal of prosthetic bilateral. Flow cytometry of liquids of seroma: without evidence of clonality. Pathological anatomy: capsule breast with granulomas by silicones.
Treatment was started with prednisolone 1mg/kg/day for two weeks and gradual decrease. Remains afebrile and normal ferritin and CRP.
Discussion
In the year 2000, a meta-analysis did not showed higher frequency of SLE, RA, scleroderma, Sjögren's, or SO combined, in women with breast implants in general or IMS4 and the FDA developed in 2011, a security report concluding that there are no studies of the association between IMS and ETC5; despite this, recently Balk et al. they found an increased risk of RA, Sjögren's syndrome and Raynaud in patients with IMS2.
In the last decade, it has been described syndromes defined by a response hi, in genetically susceptible individuals after exposure to environmental factors that act as adjuvants3. Silicone implants are biocompatible in the majority of patients, but are not immunologically inert. The leakage of silicone from the implants can cause with a certain frequency inflammation of the skin, regional lymphadenopathy and granulomatous reaction around the silicone (siliconoma), but the immune response with systemic symptoms defined as siliconosis is more rare3.
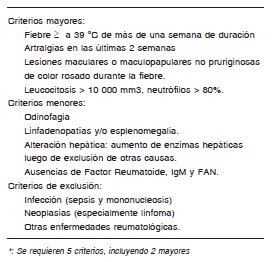
The diseases by adjuvants as siliconosis, syndrome, Gulf war syndrome, miofascitis macrophagic and phenomena post-vaccination, have been grouped by Shoenfeld and Agmon-Levine in 2010 as a syndrome autoimmune/inflammatory induced by adjuvants (ASIA). Its symptoms include myalgia, arthralgia, myositis, fever, xerostomia, and neurological symptoms6. Its diagnostic criteria are described in the Table 1. In our case, the history of leakage of the IMS, the presence of arthralgia, myalgia, fever, and the finding of siliconomas confirm syndrome of ASIA.
Table 1. Syndrome ASIA: diagnostic criteria

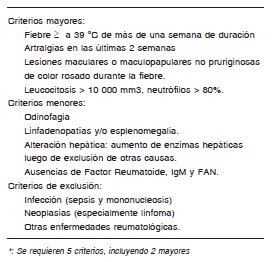
The SA start in the adult is found next to the systemic lupus erythematosus (SLE), rheumatoid arthritis (RA) and fibromyalgia, within the clinical spectrum of syndromes associated with adjuvants. According to the diagnostic criteria of Yamaguchi, the presence of fever, joint pain, enlarged lymph nodes, splenomegaly, cutaneous rash, and leukocytosis in the absence of a FAN, and rheumatoid factor, lets you diagnose in our case, SA (Table 2)7. We found in the literature, seven cases of SA side to the IMS. The time between implant placement and the onset of symptoms is variable. Patients with SA have typically a high fever, intermittent arthralgias, dark pink, lymph nodes cervical and elevation of ferritin and CRP8-13. The treatments used were mainly NSAIDS and steroids according to the severity. The removal of prosthetic was not necessary in all cases. In our patient, the presence of seroma pericapsular we bowed to the removal of the prosthesis to rule out lymphoma, anaplastic large-cell ALK ( -) - associated breast prosthesis. This entity, described by de Jong in 200814, prompted a warning from the FDA in the year 201115. The pathological anatomy of our patient to rule out this entity in the capsule and the cytometry of the content of the seroma showed no pathology clonal.
Table 2. Criteria for the diagnosis of adult Still's disease*
This case can alert physicians to suspect, of new entities linked to the presence of mammary prosthesis, such as ASIA and anaplastic large cell lymphoma ALK (-).
Christian Armenteros 1 Andrea Odzak 1 , Florence Arcondo 1 Marcela Of God Soler 2 Tatiana Sinigier 3 , Marcelo Zylberman 1
1 Clinical Medicine Division, Dr. Cosme Argerich General Acute Hospital,
2 Pathological Anatomy Service, Marie Curie Hospital,
3 Plastic Surgery, Dr. Cosme Argerich General Acute Hospital, Buenos Aires, Argentina
Summary
Connective tissue diseases associated with silicone breast implants have been a topic of discussion. In the last decade, siliconosis has been included in the adjuvant-induced autoimmune/inflammatory syndrome (ASIA) together with Gulf War syndrome, macrophagic myofasciitis syndrome and post-vaccination phenomena. ASIA can manifest as lupus, rheumatoid arthritis, or more rarely as adult-onset Still’s disease. We present the case of a patient with prolonged fever and clinical criteria compatible with ASIA and Still’s disease. The prostheses were resected and the pathology ruled out ALK (-) anaplastic lymphoma associated with prostheses. Physicians must be alert to the appearance of these new entities associated with silicone breast implants.
Keywords: ASIA syndrome; Siliconosis; Still’s disease; Adjuvant; Breast implants.
Abstract
ASIA syndrome: breast implant and Still’s disease .
Connective tissue diseases associated with silicone breast implants have been widely discussed. In the last decade, siliconosis has been included in the autoimmune/inflammatory syndrome induced by adjuvants (ASIA) next to Gulf War syndrome, macrophage myofascitis and postvaccination phenomena. The ASIA syndrome may appear as lupus, rheumatoid arthritis, or more rarely, as adult Still’s disease. We discuss the case of a patient with prolonged fever and clinical criteria for ASIA and Still’s disease. The prostheses were resected and pathology showed absence of breast implant associated anaplastic lymphoma ALK (-). Physicians should be alert to these new entities linked to silicone breast implants.
Key words: ASIA syndrome; Silicone; Still’s disease; Adjuvant; Breast implants.
Since their approval, the use of silicone breast implants (SBI) has raised suspicions of an association with connective tissue diseases (CTD) 1 . Despite recent meta-analyses and reviews, these suspicions have not been confirmed 2 . Siliconosis was one of the first diseases recognized as “adjuvant-induced” and is now included, along with others, within the Shoenfeld syndrome or adjuvant-induced autoimmune/inflammatory syndrome (ASIA) 3 . We present the case of a patient with siliconosis that manifested as adult-onset Still’s disease (AS).
Clinical Case
A 61-year-old woman was admitted for fever (39 °C), arthralgia, myalgia and pain in the anterior aspect of the left hemithorax for seven days.
She had had a breast implant replaced with silicone gel eight years ago due to prosthetic leakage. She had been hospitalized twice previously for febrile syndrome; the first, nine months ago with spontaneous resolution and the second three months before this hospitalization, when corticosteroid treatment was prescribed with normalization of the thermal curve. The following complementary tests were attached from these hospitalizations: Hct. 33%, VMC 89, GOT 84 IU/l, GPT 144 IU/l, FAL 115 IU/l, CRP (C-reactive protein) 130 mg/dl, LDH 1350 IU/l. Viral serologies, HIV, ASMA (anti-smooth muscle antibodies), anti LKM (anti-liver-kidney microsomes), FAN (antinuclear antibodies) and anti DNA negative. Complement, CPK and aldolase normal. Microbial cultures negative. CT: bilateral axillary and left supraclavicular adenomegaly > 10 mm. Splenomegaly (148 mm). Bilateral breast prosthesis with periprosthetic soft tissue thickening in the left breast. Left breast ultrasound: 28 × 6 mm anechoic collection compatible with seroma.
Left axillary lymph node biopsy: marked expansion of the T zone and foci of necrosis. Ziehl-Neelsen, PAS and Giemsa stains negative.
Liver biopsy: mild active chronic liver disease. Upper and lower video endoscopy and transesophageal echocardiogram normal.
Physical examination on admission: painless left axillary adenopathy 2 × 2.5 cm; maculopapular rash on lower limbs and trunk that worsened with fever peaks. Splenomegaly.
Laboratory: Hct. 34%, WBC 15,800/mm3, neutrophils 85%, LDH 1,581 IU/l, CRP 223 mg/l, ESR 90 mm/h, ferritin > 2,000 ng/ml, GOT 64 U/l, GPT 13 U/l. The rest, without particularities.
Chest CT scan: bilateral breast prosthesis with thickening and heterogeneity of left parasternal tissues and periprosthetic fluid. Multiple cervical, axillary and left mammary chain adenomegalies. Splenomegaly 140 mm.
Bilateral prosthesis removal was decided. Flow cytometry of seroma fluids: no evidence of clonality. Pathology: breast capsule with silicone granulomas.
Treatment with meprednisone 1 mg/kg/day for two weeks and gradual tapering was started. The patient remains afebrile and ferritin and CRP have normalized.
Discussion
In 2000, a meta-analysis found no increased incidence of SLE, RA, scleroderma, Sjögren’s, or combined CTE in women with breast implants in general or IMS4 and in 2011 the FDA issued a safety report concluding that there are no association studies between IMS and CTE5; however, Balk et al. recently found an increased risk of RA, Sjögren’s syndrome, and Raynaud’s syndrome in patients with IMS 2 .
In the last decade, syndromes defined by a hyperimmune response have been described in genetically susceptible individuals after exposure to environmental factors that act as adjuvants 3 . Silicone implants are biocompatible in most patients but are not immunologically inert. Silicone leakage from the prosthesis can frequently cause skin inflammation, regional lymphadenopathy and granulomatous reaction around the silicone (siliconoma), but the immune response with systemic symptoms defined as siliconosis is rarer 3 .
Adjuvant-induced diseases such as siliconosis, Gulf War syndrome, macrophagic myofascites syndrome and post-vaccination phenomena have been grouped by Shoenfeld and Agmon-Levine in 2010 as adjuvant-induced autoimmune/inflammatory syndrome (ASIA). Its symptoms include myalgias, arthralgias, myositis, fever, xerostomia and neurological symptoms 6 . Its diagnostic criteria are described in Table 1 . In our case, the history of IMS leakage, the presence of arthralgias, myalgias, fever and the finding of siliconomas confirm ASIA syndrome.
Table 1. ASIA syndrome: diagnostic criteria

Adult-onset AS is, together with systemic lupus erythematosus (SLE), rheumatoid arthritis (RA) and fibromyalgia, within the clinical spectrum of adjuvant-associated syndromes. According to Yamaguchi’s diagnostic criteria, the presence of fever, arthralgia, adenopathy, splenomegaly, skin rash and leucocytosis in the absence of FAN and rheumatoid factor allows us to diagnose AS in our case ( Table 2 ) 7 . We have found seven cases of AS secondary to MSI in the literature. The time between implant placement and the onset of symptoms is variable. Patients with AS typically present with intermittent high fever, arthralgia, pink macules, cervical adenopathy and elevated ferritin and CRP 8-13 . The treatments used were mainly NSAIDs and steroids depending on the severity. Prosthetic removal was not necessary in all cases. In our patient, the presence of a pericapsular seroma led us to remove the prosthesis to rule out ALK(-) anaplastic large cell lymphoma associated with breast prostheses. This entity, described by de Jong in 2008 14 , led to an FDA alert in 2011 15 . The pathology of our patient ruled out this entity in the capsule, and cytometry of the seroma contents did not show clonal pathology.
Table 2. Diagnostic criteria for adult Still’s disease*
This case may alert physicians to suspect new entities linked to the presence of breast implants, such as ASIA and ALK (-) anaplastic large cell lymphoma.
Original Source: http://www.scielo.org.ar/scielo.php?script=sci_arttext&pid=S0025-76802017000500013




