The disease for breast implants (BII, acronym in English) is a condition that is not well known, but can be debilitating. The symptoms vary from one person to another and can include fatigue, joint pain, memory and concentration problems, etc ..
The term “disease breast implants (BII)” refers to a wide variety of symptoms that occur in some people who have been subjected to reconstructive procedures, or increase aesthetic with breast implants. The BII is not a medical diagnosis officer because they still do not know her well. However, some experts believe that the symptoms of BII may be due to an inflammatory reaction or immune to the implants.
The BII can affect people that have any type of breast implant, including implants with silicone gel or saline solution, the surface smooth or textured, and round or drop-shaped. The BII can occur with implants that have been broken or that remain intact.
The BII is different to the types rare cancer that can appear in the scar tissue and in the fluid around a breast implant, as the anaplastic large cell lymphoma associated with breast implants (ALCL-AIM)other types of lymphomas and squamous cell carcinoma associated with breast implants (CCE-AIM).
Symptoms and signs of the disease for breast implants
The disease for breast implants (BII) affects everyone differently. The symptoms and signs of the disease for breast implants may include:
- muscle and joint pain
- chronic fatigue
- problems with concentration and memory
- breathing problems
- sleep disturbances
- rashes and other skin problems
- dry mouth and eye
- anxiety
- depression
- headaches
- hair loss
- gastrointestinal problems
The symptoms of the disease for breast implants may be submitted at any time after the implant surgery. Some people show symptoms immediately, while others suffer from them years later.
Many of the symptoms of BII is associated with disorders of the connective tissue and autoimmune diseases such as lupus, rheumatoid arthritis, and scleroderma. Some people with BII are also diagnosed with an autoimmune disease or disorder of the connective tissue specific, although many others do not.
In many cases, though not in all, the performance of a surgery to remove the breast implants improves or completely cure the symptoms of the disease for breast implants.
There is a diagnostic medical officer of the BII... yet.
Even though they are carrying out research studies to determine the exact cause of the BII, there is currently not an official diagnosis.
“The BII is a set of symptoms that don't fit in any other diagnosis classic of disease,” he says Diana Zuckerman, PhD, president of the National Center for Research on Health in the united States and researcher who studies the safety problems associated with breast implants. “We believe that, with time, will be recognized as a ‘medical condition’, but that process will take time.”
The Food and Drug Administration (FDA), the associations of plastic surgery to be more important and other health authorities to come paying more attention to the BII than before. In October 2021, the FDA began to require manufacturers of breast implants include information on the risk of symptoms that affect the entire body in a special warning printed on the container of breast implants and a checklist for decision making included in the information leaflets for patients. 1 The FDA refers to symptoms that affect the entire body, rather than a single organ or a body part-specific, such as systemic symptoms. The FDA announced that it will restrict the sale and distribution of breast implants only to the health care professionals to review the checklist as part of the process of informed consent prior to the surgery, but it is not clear how to apply this.
In addition, the American Society of Plastic Surgeons, the Foundation for Education and Research in Cosmetic Surgery and the Foundation of Plastic Surgery are developing and funding new research studies on the BII.
How common is the disease for breast implants?
It is not entirely clear how many people that have breast implants suffering from BII. During the past few years, more people report to their doctors and the FDA on symptoms of BII. Some of the doctors and other experts with whom we spoke noted that the groups in social networks and the coverage of the media have helped to raise awareness of the condition. There are many online communities related to the disease for breast implants, and some of them have tens of thousands of members.
Analysis and diagnosis of the disease by breast implants
Currently, there are no tests or diagnostic criteria in common use specifically for the BII.
Plastic surgeons specialized in the treatment of BII affirm the following:
- It is common for people who seek therapy present a variety of symptoms that interfere with your ability to function.
- Many people have consulted with several doctors before realizing that the symptoms may be related to breast implants.
“Usually, my patients with BII I found after exhausting all other avenues of medical and after undergoing extensive testing,” says the Dr. Robert Whitfield, md, FACS, a plastic surgeon who treats people suffering from BII and who was president during 2019 of the Foundation for Education and Research in Cosmetic Surgery.
Because there is an analysis that allows to confirm a diagnosis of BII, plastic surgeons may need to ask for analysis and review medical records to rule out other diseases or conditions that could be the cause of the symptoms. It is possible that physicians need to do tests to detect arthritis, Lyme disease, or thyroid problems, for example, and see if the symptoms improve with treatment of these conditions. In some cases, someone may have, BII, and, at the same time, an autoimmune disease diagnosed or other conditions.
Treatment of disease by breast implants
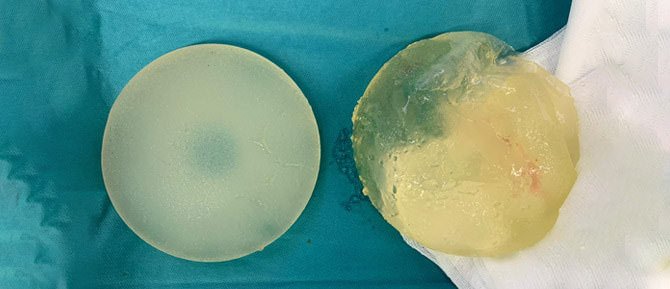
Plastic surgeons who have experience in the treatment of BII to those who consulted stated that extract the implants and to remove the entire or a part of the capsule of scar tissue around them is the most effective treatment to improve long-term symptoms. One of the procedures that tend to practicing surgeons is called capsulectomy total.
In a study published in the journal Aesthetic Surgery Journal in December of 2021, and in several other studies, we showed that people who had reported cases of BII often present a significant improvement of their symptoms of BII after surgery to remove breast implants and remove the capsule of scar tissue. 2 Doctors and scientists do not yet know exactly why the symptoms of BII often improve after the removal of implants.
In general, the plastic surgeons do not recommend replacing the implants with new ones if you have symptoms of BII. There is a risk that reappear the symptoms of BII. After that I removed the implants, and depending on your situation and preferences of each individual, maybe you'll decide stay flat or take a breast reconstruction with flaps (reconstruction weld), fat autografting, or both options.
If you are considering to submit to a surgery to treat the symptoms of BII, be sure to consult with the plastic surgeon about the risks and benefits of the different approaches of surgical treatments.
It is possible that the removal of breast implants does not necessarily improve or resolve symptoms of BII.
In addition, ask the surgeon whether to recommend to send you samples of the capsule of scar tissue and the liquid extracted during the surgery to a lab for analysis, pathological, and crops.
Some doctors say that it can be helpful to eat healthier, exercise regularly, and reduce stress after the surgery to remove the implants after the diagnosis of BII. Follow these tips, you can promote healing and decrease inflammation-related symptoms of BII.
New research about the disease through breast implants
Most of the information of existing scientific does not show a defined relationship between breast implants and autoimmune diseases or connective tissue, and also shows that breast implants cause these conditions. According to a pair of recent studies, breast implants, silicone gel-filled are associated with a slightly higher risk of developing an autoimmune disease or connective tissue. One of the reasons why these studies are worthy of note is that each one included a large number of women who were followed up for a period greater than that of the majority of the previous studies on the safety outcomes in women with breast implants.
In a study published online in the journal Annals of Surgery in September 2018, a research team at MD Anderson Cancer Center the University of Texas examined the clinical records of 99.993 women who had implants and who were enrolled in studies on long-term security required by the FDA. 3The researchers found that, compared with women in the general population, women with implants, silicone gel-filled were eight times more likely to receive a diagnosis of Sjögren's syndrome, an autoimmune disease that is characterized by dryness of the eyes and mouth; seven times more likely to receive a diagnosis of scleroderma (a group of autoimmune diseases that cause the skin and connective tissues to harden and tighten), and about six times more likely to receive a diagnosis of rheumatoid arthritis.
The study had some weaknesses. Some of the illnesses reported by the people that participated were not necessarily diagnosed by a doctor, and a significant amount of people left the study before the end.
In a study published online in the journal International Journal of Epidemiology in October 2018, a team of researchers examined the electronic medical records of 123.255 women israelis (24.651 had breast implants, silicone gel-filled, while the rest did not have breast implants). 4 The medical records contained up to 20 years of data. The researchers found that women with breast implants, silicone gel-filled were significantly more likely to receive a diagnosis of autoimmune disorders or rheumatic, such as Sjögren's syndrome, systemic sclerosis and sarcoidosis, compared with women without breast implants in a range of age and socio-economic level is similar.
What can you mean all this for you?
If you are thinking to replace your breast implants or to place implants for the first time, talk to your plastic surgeon and other physicians about all of the benefits and risks, including the risk of suffering from BII.
If you think that you have BII, it may be a good idea to find a board-certified plastic surgeon who has experience in treating people with this condition, or at least a plastic surgeon that you take seriously your concerns and don't downplay your symptoms. Keep in mind that the surgeon that you placed the implants should not necessarily be who you choose to quitártelos.
In most cases, insurance plans, private medical cover surgery to remove the breast implants in women who underwent a mastectomy and breast reconstruction. Given that there is a diagnostic code official for the BII, plastic surgeons usually listed symptoms, such as pain, rupture of the implant, and shortness of breath in order to show the insurance company that the surgery is medically necessary. It is possible that you may have to pay for the removal of implants for its own account if the plastic surgeon does not accept your health care plan or if it is considered by out-of-network care.
Read more about the BII in our Special report: disease breast implants and ALCL-AIM.
Get information on the other risks and complications after breast reconstruction with implants.
Breast implant illness (BII) is a condition that is not widely known, but can be debilitating. Symptoms vary from person to person and can include fatigue, joint pain, concentration and memory problems, etc.
The term “breast implant illness” (BII) refers to a wide variety of symptoms that occur in some people who have undergone cosmetic reconstruction or augmentation procedures with breast implants. BII is not an official medical diagnosis because it is not well understood. However, some experts believe that the symptoms of BII may be due to an inflammatory or autoimmune reaction to the implants.
BII can affect people with any type of breast implant, including those filled with silicone gel or saline, those with smooth or textured surfaces, and those that are round or teardrop-shaped. BII can occur with implants that have ruptured or that remain intact.
BII is different from rare types of cancer that can develop in the scar tissue and fluid around a breast implant, such as breast implant- associated anaplastic large cell lymphoma (BIA-ALCL) , other types of lymphomas, and breast implant-associated squamous cell carcinoma (BISA-SCC).
Symptoms And Signs Of Breast Implant Illness
Breast implant illness (BII) affects everyone differently. Symptoms and signs of breast implant illness may include:
- joint and muscle pain
- chronic fatigue
- concentration and memory problems
- respiratory problems
- sleep disorders
- Skin rashes and other skin problems
- dry mouth and eyes
- anxiety
- depression
- Headaches
- hair loss
- Gastrointestinal disorders
Symptoms of breast implant illness can occur at any time after implant surgery. Some people experience symptoms immediately, while others experience them years later.
Many of the symptoms of BII are associated with connective tissue disorders and autoimmune diseases, such as lupus, rheumatoid arthritis, and scleroderma. Some people with BII are also diagnosed with a specific autoimmune disease or connective tissue disorder, although many others are not.
In many, but not all, cases, surgery to remove breast implants improves or completely cures the symptoms of breast implant illness.
There is no official medical diagnosis for BII…yet.
Although research studies are being conducted to determine the exact cause of BII, there is currently no official diagnosis.
“BII is a collection of symptoms that don’t fit into any other classic disease diagnosis,” says Diana Zuckerman, PhD , president of the National Center for Health Research and a researcher who studies safety issues related to breast implants. “We think it will eventually be recognized as a ‘medical condition,’ but that process will take time.”
The Food and Drug Administration (FDA), major plastic surgery associations, and other health authorities are paying more attention to BII than ever before. In October 2021, the FDA began requiring breast implant manufacturers to include information about the risk of body-wide symptoms in a special warning printed on breast implant packaging and in a decision-making checklist included in patient information leaflets. 1 The FDA refers to symptoms that affect the entire body, rather than a single organ or specific body part, as systemic symptoms . The FDA announced that it will restrict the sale and distribution of breast implants only to health care professionals who review the checklist as part of the informed consent process before surgery, but it is unclear how this will be enforced.
Additionally, the American Society of Plastic Surgeons, the Aesthetic Surgery Education and Research Foundation, and the Plastic Surgery Foundation are developing and funding new research studies on BII.
How Common Is Breast Implant Illness?
It’s not entirely clear how many people who have breast implants have BII. In recent years, more people are reporting symptoms of BII to their doctors and the FDA. Some of the doctors and other experts we spoke to said social media groups and media coverage have helped raise awareness of the condition. There are many online communities related to breast implant illness, some with tens of thousands of members.
Analysis And Diagnosis Of Breast Implant Disease
Currently, there are no commonly used diagnostic tests or criteria specifically for BII.
Plastic surgeons specializing in the treatment of BII say the following:
- It is common for people seeking treatment to present several symptoms that interfere with their functional ability.
- Many people have consulted several doctors before realizing that their symptoms may be related to breast implants.
“My BII patients typically find me after exhausting all other medical avenues and undergoing extensive testing,” says Robert Whitfield, MD, FACS , a plastic surgeon who treats people with BII and was the 2019 president of the Foundation for Cosmetic Surgery Education and Research.
Because there is no test that can confirm a diagnosis of BII, plastic surgeons may need to order tests and review medical records to rule out other diseases or conditions that could be causing symptoms. Doctors may need to test for arthritis, Lyme disease, or thyroid problems, for example, and see if symptoms improve with treatment for those conditions. In some cases, someone might have BII and a diagnosed autoimmune disease or other conditions at the same time.
Treatment Of Breast Implant Illness
Plastic surgeons who have experience treating BII and whom we consulted said that removing the implants and removing all or part of the scar tissue capsules surrounding them is the most effective treatment for improving symptoms in the long term. One of the procedures surgeons often perform is called a total capsulectomy .
A study published in the Aesthetic Surgery Journal in December 2021, and several other studies, showed that people who had reported BII often had significant improvement in their BII symptoms after surgery to remove breast implants and ablate scar tissue capsules. 2 Doctors and scientists still don’t know exactly why BII symptoms often improve after implant removal.
Plastic surgeons generally do not recommend replacing your implants with new ones if you have symptoms of BII. There is a risk that your BII symptoms will return. After your implants are removed, and depending on your particular situation and preferences, you may decide to remain flat or undergo breast reconstruction with flaps (autogenous reconstruction) , fat grafting , or both.
If you are considering surgery to treat the symptoms of BII, be sure to discuss the risks and benefits of different surgical treatment approaches with your plastic surgeon.
Removing breast implants may not necessarily improve or resolve BII symptoms.
Also, ask your surgeon if he or she recommends sending samples of the scar tissue capsule and fluid removed during surgery to a laboratory for pathology and culture analysis.
Some doctors say that eating a healthy diet, exercising regularly, and reducing stress after surgery to remove implants following a diagnosis of BII can be helpful. Following these tips can promote healing and reduce inflammation related to BII symptoms.
New Research On Breast Implant Illness
For the most part, existing scientific information does not show a definitive link between breast implants and autoimmune or connective tissue diseases, nor does it show that breast implants cause these conditions. A pair of recent studies have found that silicone gel-filled breast implants are associated with a slightly higher risk of autoimmune or connective tissue disease. One reason these studies are notable is that each included a large number of women who were followed for a longer period than most previous studies of safety outcomes in women with breast implants.
In a study published online in the Annals of Surgery in September 2018, a research team at the University of Texas MD Anderson Cancer Center examined the medical records of 99,993 women who had implants and were enrolled in long-term safety studies required by the FDA. 3 The researchers found that compared with women in the general population, women with silicone gel-filled implants were eight times more likely to be diagnosed with Sjögren’s syndrome, an autoimmune disease characterized by dry eyes and mouth; seven times more likely to be diagnosed with scleroderma (a group of autoimmune diseases that cause skin and connective tissues to harden and tighten); and nearly six times more likely to be diagnosed with rheumatoid arthritis.
The study had some weaknesses. Some of the illnesses reported by the people who participated were not necessarily diagnosed by a doctor, and a significant number of people dropped out of the study before it was finished.
In a study published online in the International Journal of Epidemiology in October 2018, a team of researchers examined the electronic medical records of 123,255 Israeli women (24,651 had silicone gel-filled breast implants, while the remainder did not have breast implants). 4 The medical records contained up to 20 years of data. The researchers found that women with silicone gel-filled breast implants were significantly more likely to be diagnosed with autoimmune or rheumatic disorders, such as Sjögren’s syndrome, systemic sclerosis, and sarcoidosis, compared with women without breast implants in a similar age range and socioeconomic status.
What Can All This Mean For You?
If you are considering replacing your breast implants or getting implants for the first time, talk to your plastic surgeon and other doctors about all the benefits and risks, including the risk of BII.
If you think you have BII, it may be a good idea to find a board-certified plastic surgeon who has experience treating people with this condition or at least a plastic surgeon who will take your concerns seriously and not downplay your symptoms. Keep in mind that the surgeon who placed your implants may not necessarily be the one you choose to remove them.
In most cases, private health insurance plans cover surgery to remove breast implants in women who have had a mastectomy and breast reconstruction. Since there is no official diagnostic code for BII, plastic surgeons typically list symptoms such as pain, implant rupture, and shortness of breath to prove to the health insurance company that the surgery is medically necessary. You may have to pay for implant removal out of your own pocket if the plastic surgeon does not accept your health plan or is considered out-of-network.
Read more about BII in our Special Report: Breast Implant Illness and ALCL-AIM .
Learn about other risks and complications after breast reconstruction with implants .
Written by Jen Uscher
It was last updated on February 7, 2024
Original Source: https://www.breastcancer.org/es/tratamiento/cirugia/reconstruccion-mamaria/tipos/implante-reconstruccion/enfermedad/enfermedad-implante-mamario